Peripheral neuropathy is nerve damage most often felt in the body’s extremities. It occurs along the peripheral nerves that carry signals between the brain and spinal cord to the muscles, skin, and internal organs. When it first develops, people often report an itching, tingling or prickling in the toes or feet and perhaps legs. The fingers, hands and arms can also be affected.
In the United States, peripheral neuropathy is common and is caused most often by diabetes and alcoholism; but it’s also common in people with HIV. When diagnosed and treated early, peripheral neuropathy can often be controlled. For some, though, managing it can be challenging especially in older individuals where it’s more common.
What causes peripheral neuropathy?
Peripheral nerves are not protected by bone like the spinal chord and brain, which leaves them open to possible injury and infection. This can happen to the nerve cell body, the nerve fiber or even its coating. Direct injury, such as a broken bone or a severe burn, can damage these nerves. Certain diseases (such as diabetes, arthritis or lupus) and certain infections (such as CMV and herpes) can also damage the nerves. Finally, certain medicines and an imbalance of some vitamins can cause this condition.
HIV itself has also been shown to cause nerve damage, usually in people with seriously damaged immune systems. Though researchers aren’t certain how HIV causes this type of injury, many believe it is due to the chronic inflammation that’s present in the immune system.
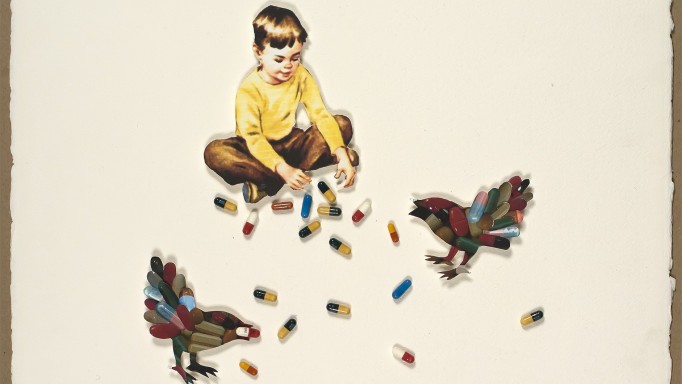
Earlier HIV meds contributed to the condition, along with some drugs commonly used for AIDS-related infections. This may be due to the drugs damaging small structures inside cells (mitochondria) that provide energy to the cell. However, newer HIV meds have not shown this risk, although it may take many more years before it appears.
Who is at risk?
Several risk factors put people with HIV at higher risk for peripheral neuropathy. These include a history of the condition, higher viral load, CD4 count below 100, an AIDS-defining condition, use of drugs that damage nerves, diabetes, poor nutrition (too little vitamin B12 or E or too much B6), and heavy use of alcohol.
Men and women seem to have the condition at about the same rate. Peripheral neuropathy more often appears in later stage HIV disease and in older individuals. The risk greatly increases as two or more of the drugs listed above are used together, and especially if they’re used in people with any of the above conditions.
Some drugs that may increase the risk of peripheral neuropathy include:
- Hivid (zalcitabine) – no longer used in the U.S. for HIV treatment
- Videx; Videx EC (didanosine) – no longer used in the U.S. for HIV treatment
- Zerit (stavudine) – no longer used in the U.S. for HIV treatment
- Nydrazid (isoniazid) – prevention and treatment of tuberculosis (TB)
- Oncovin (vincristine) or Velban (vincristine) – treatment for Kaposi sarcoma (KS)
- Myambutol (ethambutol) – treatment for MAC and other bacterial infections
- Flagyl (metronidazole) – treatment for amoebas and parasitic infections
- Zyvox (linezolid) – treatment for bacterial infections
- Dapsone – treatment for PCP and other infections
What are the symptoms of peripheral neuropathy?
Symptoms vary from person to person and can range from mild to severe and perhaps disabling. Sometimes neuropathy is present even without symptoms. They can appear suddenly, come and go, or persist over time. They usually affect both sides of the body at the same time, and they may get worse at night.
If you experience any of the following in your toes, feet, fingers or hands, talk to your doctor so you can find the source of these symptoms and create a treatment plan.
- Tingling, pinching, prickling or buzzing sensation
- Cramping, burning, throbbing or shooting pain
- Feeling “frostbite”, “pins and needles”, “a lit match” or “walking on broken glass”
- Numbness to pain or temperature
- Extreme sensitivity to touch Loss of balance/coordination
- Loss of reflexes (your doctor can check these)
- Muscle weakness
- Noticeable changes in the way you walk or move
- Having to urinate more during the day and at night
- Difficulty walking up and down stairs
- Stumbling or falling
- Erectile dysfunction
What is the treatment for peripheral neuropathy?
It may take some time to discover the underlying cause(s) for your peripheral neuropathy and to treat it properly. Generally speaking, the best way to manage peripheral neuropathy is to stop (or switch) any medications that may be causing the problem in consultation with your doctor. It can sometimes take a few weeks or months for symptoms to improve after stopping, switching or adjusting the dose of an offending drug. In some cases, symptoms can worsen before they get better.
If treating the underlying cause isn’t possible, it is still likely that the symptoms can be treated to hep relieve the pain. Here are some treatemnts that can help reduce the symptoms of peripheral neuropathy:
- Non-narcotic pain relievers. Acetaminophen (Tylenol, etc.), aspirin, ibuprofen (Advil, etc.), and naproxen (Aleve, etc.) can help ease mild-to-moderate pain. They’re available over-the-counter and by prescription. While they can irritate the stomach, they are not addictive and can be taken regularly to maintain comfort.
- Narcotic pain relievers. These prescription meds can help ease moderate-to-severe pain and can be used together with non-narcotic pain relievers, tricyclic antidepressants or anticonvulsants. Side effects can include nausea, vomiting, constipation, tiredness and sleepiness. For those with a history of drug addiction, taking a short-term course of these should be safe, but discuss this with your doctor. Low doses of some of these drugs should be started at first and then gradually increased until the pain is more manageable. Also, these drugs may interact with HIV drugs.
- Topical medications. Lidoderm (5% lidocaine gel) is a prescription anesthetic gel applied directly to the skin. Although some people use it, one study with 65 HIV-positive people did not show that it reduced the pain caused by peripheral neuropathy. Alternatively, a skin patch with capsaicin (the compound that makes chili peppers “spicy”) is available as Qutenza and is approved for reducing the pain of a shingles outbreak. The ASCEND study of 429 people with peripheral neuropathy that included some people with HIV showed it moderately reduced pain.
- Tricyclic antidepressants. These drugs work by adjusting the balance of certain chemicals in the brain, called “neurotransmitters”. But they also inhibit certain cell receptors, which cause their many possible side effects. Tricyclic antidepressants are normally given in small increasing doses to avoid side effects, giving the body a chance to adapt. Common side effects include dry mouth and nose, blurred vision, drowsiness, difficult urination and constipation, among many others. These drugs are usually used to treat mild-to-moderate pain, and are sometimes taken with non-narcotic and narcotic pain relievers. However, studies actually show that tricyclic antidepressants are not clinically effective even though some people report that their symptoms improve. The more common drugs used for peripheral neuropathy include Elavil (amitriptyline), Aventyl (nortriptyline), Norpramin (desipramine) and Tofranil (imipramine). Some HIV medicines can change the blood levels of tricyclic antidepressants.
- Anticonvulsants. These drugs work by controlling the nerve activity in the brain and are used to treat epilepsy. They’re being used more often to treat other conditions like peripheral neuropathy, and studies show some success in controlling its pain. Several are used: Dilantin (phenytoin), Lamictal (lamotrigine), Lyrica (pregabalin), Neurontin (gabapentin), Tegretol (carbamazepine) and Topamax (topiramate). Anticonvulsants are usually given in small increasing doses to avoid side effects, giving the body a chance to adapt. Common side effects include drowsiness, dizziness, nausea, vomiting and constipation. Others include rash, restlessness, sleep problems, memory problems, sore joints or muscles, among many others. Care must be taken with possible drug interactions with some HIV meds.
- Cannabis (marijuana). A 2007 study report showed that smoking medical marijuana reduced chronic pain due to peripheral neuropathy in just over half of its 50 adult volunteers. All smoked 3 cigarettes a day for 5 days, half with medical marijuana vs. half with placebo. The amount of relief averaged a more than a 30% reduction in pain. Side effects included dizziness, anxiety, confusion and sedation.
- Acupuncture. Some people report that acupuncture helps them to manage their pain. Research has not proven this effective. However, a person’s belief in the process may be enough for her or him to get relief.
What can I do to help control the pain?
Some people find that a single change in lifestyle is enough while others use several ways to ease their discomfort.
- Wear proper shoes. Tight or ill-fitting shoes can cause pain, so consider wearing shoes that give the proper support for your feet while still being flexible. Consult a foot doctor or experienced salesperson.
- Keep your hands/feet cool. Soaking your feet and hands in cold water can help reduce the pain. Keep your feet and hands free of bed covers at night.
- Improve your diet. Foods high in B12 include liver, snapper, salmon, beef, poultry, milk, eggs, shellfish, tofu and yeast. Foods with E include green leafy vegetables, carrots, nuts, oils (olive, corn, canola, safflower, sunflower), wheat germ, whole grains, and margarines made from plant oils. Consider supplements.
- Get a massage. Massaging your feet and hands increases blood flow, which can ease pain and help you relax. A massage therapist or friend can also help.
- Avoid strain. Ease pain by not walking great distances or standing for long periods. Avoid repetitive tasks with your hands and fingers. On the other hand, moderate walking can help improve blood flow and reduce symptoms.
- Use support tools. Many of the aids that help older adults with their mobility concerns can be found in stores and online. Kitchen tools are available with easy grips as well as reachers for items on shelves. Dressing aids are also available, from long-handled shoehorns and brushes to zipper pulls and elastic shoestrings.
Last Reviewed: February 2, 2022