In order for your health care team to know how best to care for you and manage your HIV, blood tests should be done on a regular basis. With today’s effective and well-tolerated antiretroviral treatment, people living with HIV no longer require monitoring as often as they used to. But it’s still important to get the recommended tests to keep tabs on your overall health and make sure your treatment is still working well.
Here are the tests you will need:
This test measures the number of copies of HIV’s genetic material in a small amount of blood. Two types of HIV genetic material may be measured, RNA or DNA. RNA tests are usually used for routine blood monitoring, but DNA tests can sometimes detect hidden HIV even if an RNA test is undetectable.
There is no normal range for viral load—the point of HIV treatment is to keep it as low as possible for as long as possible. Standard HIV RNA viral loads tests usually can measure down to 50 or sometimes 20 copies. If your result comes back “not detected” or “undetectable,” your viral load is very low, known as viral suppression. Some tests used for research are more sensitive and can measure down to a single copy.
Viral load tests are used to monitor how well HIV treatment is working and whether it’s time to switch to a new regimen. When starting treatment, certain HIV medications are not recommended for people with a high viral load above 100,000 copies. Some treatment combinations, known as maintenance therapy, are only recommended for people who are switching medications after they already have an undetectable viral load.
Department of Health and Human Services (DHHS) guidelines recommend getting a viral load test when you first seek care for HIV, when antiretroviral treatment is started or modified and again at two to eight weeks after starting or switching therapy. If viral load is detectable at that point, testing should be repeated every four to eight weeks until it falls below 200. After that, viral load should be monitored every three to six months. Viral load should also be tested if treatment appears to be failing or if clinically indicated.
Once a person is on treatment and has achieved viral suppression, viral load can rise again for a few reasons.
Sometimes an occasional, temporary rise called a “blip” can occur. This could be due to a lab error or indicate that a person has another infection, but often there is no known reason. This is usually nothing to worry about.
However, a trend of increasing viral load over time is a bigger concern. This could mean a person is struggling with adherence or having trouble getting refills consistently. It could also mean that a drug interaction is preventing HIV meds from fully controlling the virus. In any case, this should be discussed and resolved with your health care provider.
Increasing viral load over time can also mean that HIV has developed resistance to one or more drugs in the regimen. If this happens, it’s important to get a drug resistance test done; these tests are most accurate when viral load is at least 1,000 copies. Genotypic tests, which analyze viral genetic sequences, are most commonly used; phenotypic tests look what happens when HIV is exposed to a drug in a laboratory. If resistance is detected, it may be time to change your regimen to include drugs that can fully suppress HIV.
Here’s what a viral load test report looks like:
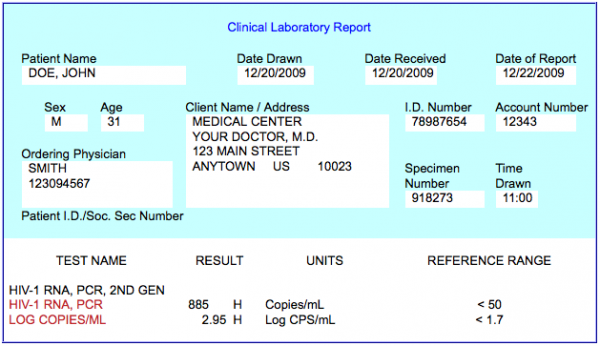
HIV-1 RNA
The number of copies ofHIV RNA found by the test. HIV-1 is the most common type ofHIV seen in the U.S. (HIV-2 is usually found in West and Central Africa.) Three testing techniques may be used: RT-PCR (or simply PCR), branched DNA (bDNA) or NASBA.
Log Copies/mL
A “log” is a term scientists use to refer to amounts; in this case, it is copies of HIV RNA. In the simplest terms, 1 log represents one “0”. Therefore, 2 log means 100 copies, 3 log means 1,000 copies (or more accurately 10 x 10 x 10), etc. Logs are also used to measure changes in viral load. For example, a viral load that goes from 100,000 down to 100 is a 3-log reduction.
A CD4 T cell is a type of immune system white blood cell. These cells coordinate the activities of other immune system cells that fight viruses, bacteria and cancer.
HIV prefers to enter CD4 cells in order to multiple. This kills the cells, causing their number to decrease over time. Having too few CD4 cells means that the immune system will no longer function as it is should, leaving people prone to opportunistic illnesses.
Several types of white blood cells carry out immune responses. These include two types of lymphocytes: B cells and T cells. Both are made in the bone marrow, but B cells stay there to mature while T cells move the thymus to mature. B cells produce antibodies, which help fight harmful invaders such as bacteria, viruses and fungi.
T cells are divided into three groups:
- Helper T cells (T4 or CD4 cells) coordinate the activity of other types of immune cells.
- Killer T cells (a type of CD8 cell) recognize and destroy abnormal cells, such as cancer cells and cells infected with viruses.
- Suppressor T cells (another type of CD8 cell) limit the activity of other immune cells so they don’t harm normal tissue.
Getting regular CD4 counts will show how healthy your immune system is and whether your antiretroviral treatment is working. CD4 levels were previosuly used to decide when to start treatment, but now antiretroviral therapy is recommended for everyone diagnosed with HIV regardless of CD4 count. People with a very low CD4 count may need additional medications to prevent AIDS-related illnesses.
DHHS guidelines recommend getting a CD4 test every three to six months during the first two years on treatment, if your viral load rises while on treatment or if your CD4 count is below 300. After you’ve been on treatment with stable viral suppression for two years, CD4 tests can be done once a year if your count is between 300 and 500, or skipped entirely if it’s above 500.
The following is an example of a lab report for T cell measurements. The numbers represent the amounts found in a small drop of blood called a cubic millimeter. You will usually see a range of numbers listed for each test result, so you can compare your numbers to the normal range for most HIV-negative people.

CD3 Absolute Count
The number of all T cells, which includes CD4 and CD8 cells. This figure is rarely used for making treatment decisions.
CD3 Percentage
The proportion of all immune cells that are T cells. This figure is also rarely used for making treatment decisions.
CD4 Cell Count
The absolute number of CD4 cells. The normal range for an HIV-negative person is 500 to 1,500. The goal of HIV treatment is to keep this number as high as possible for as long as possible. A CD4 count below 200 indicates an AIDS diagnosis and raises the risk for opportunistic illnesses.
CD4 Percentage
The CD4 percentage, or the proportion of all T cells that are CD4 cells. This may be more reliable because it tends to vary less than the absolute CD4 count. The normal range for HIV-negative adults is 30% to 60%; people with HIV often have a lower percentage. A percentage below 14% indicates an AIDS diagnosis. CD4 percentage, rather than CD4 count, is used to monitor disease progression in children.
CD8 Cell Count
The absolute number of all CD8 cells, which include both killer and suppressor T cells. The normal range for an HIV-negative person is 150 to 1,000. It is usually higher in people with HIV. This figure is rarely used for making treatment decisions.
CD8 Percentage
The proportion of all T cells that are CD8 cells. The CD8 percentage is sometimes more reliable because it tends to vary less than the CD8 count.
CD4/CD8 Ratio (helper cell/suppressor cell ratio)
The CD4/CD8 ratio, or the CD4 count divided by the CD8 count, gives a fuller picture of immune system health. The normal range for HIV-negative people is around 1.0 to 4.0, or one to four CD4 cells for every CD8 cell. People with uncontrolled HIV may have fewer CD4 cells than CD8 cells, indicated by a ratio less than 1.0.
A chem screen reports the amounts of various chemicals in the blood. While it doesn’t really tell you much about HIV or the health of your immune system, it can reveal a lot about your overall health, including metabolic status and liver or kidney problems. Several of these measurements could indicate drug side effects.
DHHS guidelines recommend getting a basic chem screen when you first seek HIV care, when you start or switch treatment and again at two to eight weeks after starting or switching therapy. After that, these tests can be done every six months or whenever clinically indicated. If your doctor does glucose and lipid (blood fat) testing separate from the chem screen, these can be done every year.
Here’s what a chemscreen report looks like:

Glucose
The food you eat is processed into glucose (blood sugar), fats (lipids) and proteins in the body. Glucose levels in the blood are most reliably measured after fasting, for example in the morning before eating.
Cholesterol and Triglycerides
Lipids include triglycerides and cholesterol, which in turn is broken down into low-density lipoprotein (LDL), known as “bad” cholesterol, and high-density lipoproteins (HDL), or “good” cholesterol. Having elevated triglycerides and LDL is a risk factor for cardiovascular disease, while a high HDL level is protective. Having a higher proportion of HDL relative to total cholesterol, known as the total cholesterol/HDL ratio, is better. Some HIV meds can alter triglyceride and cholesterol levels.
Electrolytes
Sodium, potassium, chloride, bicarbonate, phosphate, calcium and magnesium are all electrolytes—the charged particles that make up a salt. Electrolytes play a crucial role in maintaining the body’s pH (acidity level), and they affect various cell functions and the electrical activity of the heart. Abnormal electrolyte levels may result from persistent diarrhea or vomiting or chronic conditions such as kidney dysfunction.
Iron
Iron is an important mineral that is a component of hemoglobin, the protein in red blood cells that transports oxygen to all cells and tissues in the body. A low level can be a sign of anemia or internal bleeding and should be followed up by a health care provider.
Blood Proteins
Albumin and globulin are the two types of protein included in the total protein measurement. Albumin is a blood protein that helps maintain the fluid balance in the bloodstream. Globulins play a role in liver function, blood clotting and immune function. One type, immunoglobulins—better known as antibodies—fight infections. The albumin/globulin, or A/G ratio, reflects the amount of albumin relative to the amount of globulin in the blood. Some people with HIV have below-normal A/G ratios, though this usually isn’t anything to worry about, as long as albumin levels are normal.
Kidney Biomarkers
BUN (Blood Urea Nitrogen), creatinine and uric acid are waste products in your blood and urine. Because your kidneys excrete these wastes into your urine, levels in the blood are used to monitor kidney function. Many drugs, including some HIV meds, can affect BUN and creatinine levels and the BUN/creatinine ratio.
Liver Biomarkers
Bilirubin (total and direct), alkaline phosphatase, gamma-glutamyl transferase (GGT), alanine transaminase (ALT) and aspartate transaminase AST) are enzymes produced by the liver. Elevated levels can indicate liver problems, which may be due to medication side effects, viral hepatitis, fatty liver disease or other causes. Elevated bilirubin can cause the skin and eyes to look yellowish, a condition known as jaundice.
Other Biomarkers
Amylase is a digestive enzyme produced by the salivary glands and pancreas. An elevated level, which can indicate swelling or inflammation of the pancreas (pancreatitis), is side effect of some older HIV meds. LD or LDH stands for lactate dehydrogenase, an enzyme involved in energy production. An elevated level can indicate acute or chronic tissue damage and, along with other lab tests, it may help diagnose liver disease, pancreatitis, certain cancers or other problems.
One of the most important blood tests that your doctor will order is a complete blood count (CBC), an inventory of different types of blood cells. These can be grouped into three categories: red blood cells, white blood cells and platelets. Knowing how many of these cells are in a blood sample provides a lot of valuable information.
DHHS guidelines recommend a CBC when you first seek HIV care, when you start or switch treatment and then every three to six months, along with a CD4 count. If you are on stable treatment and your CD4s are no longer being monitored regularly, get a CBC every year or if clinically indicated.
Here’s what a CBC report looks like. The reference ranges shown below are for adult men. Some may vary for women, children and adolescents. Check your lab report for specific reference ranges.

White Blood Cells (WBC)
White blood cells, or leukocytes, are immune system cells that defend the body against invaders and cancers. They are formed in bone marrow and either enter the blood or migrate to key organs such as the spleen, lymph nodes or gut. White blood cells include lymphocytes, neutrophils and monocytes. Some CBC reports include a differential section that breaks out their numbers and percentages. B cells and T cells (CD4 and CD8 cells) are types of lymphocytes, but they are not typically broken out in a standard CBC report; for that, you will need a CD4 count (described above). A high WBC count may indicate that an infection is present, while a low number might indicate that an infection or disease—such as HIV or cancer—has reduced the bone marrow’s ability to produce new cells; some drugs also cause bone marrow damage.
Red Blood Cells (RBC)
Red blood cells, or erythrocytes, are responsible for delivering oxygen throughout the body. Healthy people typically have between 3 and 6 million of these cells in a milliliter of blood. A low RBC count can indicate anemia, which can lead to fatigue. Some older HIV meds, as well as some AIDS-related infections and cancers, can cause anemia. A high RBC count may occur in people with low oxygen levels, for example due to heart disease or chronic lung disease.
Hemoglobin (HGB) and Hematocrit (HCT)
Hemoglobin and hematocrit provide more information about red blood cells. Hemoglobin is the protein in red blood cells that transports oxygen. Hematocrit refers to the proportion of blood that is made up of red blood cells. For men, the hematocrit should be between 40% and 52%; for women, it should be between 35% and 46%. A low hemoglobin level or hematocrit percentage may indicate anemia.
Mean Corpuscular Volume (MCV)
This test measures the size of red blood cells. Larger red blood cells may indicate anemia due to vitamin B6 or folic acid deficiency while smaller red blood cells may indicate anemia due to iron deficiency. Some older HIV meds can cause changes in MCV.
Mean Corpuscular Hemoglobin (MCH) and Mean Corpuscular Hemoglobin Concentration (MCHC)
These tests measure the amount of hemoglobin in red blood cells. Low levels indicate anemia.
Red Cell Distribution Width (RDW)
Since red blood cells can come in different sizes, RDW looks at the range of these sizes in a blood sample. If anemia is suspected, RDW test results are often used together with MCV to figure out what the cause might be.
Platelets
Platelets are tiny cell fragments that enable the blood to clot in case of injury, but excessive clotting can lead to blockage of arteries or veins. A high platelet count might be seen in people with certain types of cancer, rheumatoid arthritis or inflammatory conditions. A low platelet count, called thrombocytopenia, is often seen in people with HIV, liver disease and certain types of cancer. It may occur as a side effect of drugs that damage the bone marrow. Thrombocytopenia can lead to bleeding and bruising. It’s important
to determine the underlying cause in order to correct it.
Last Reviewed: March 1, 2023